Your body can contract several infections from bacteria. Knowing the warning signs and symptoms of bacterial infections is crucial since they can develop into catastrophic conditions if left untreated. Schedule a visit with your doctor if you believe you have a bacterial illness. You will feel better more quickly if you seek therapy right away.
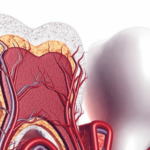
The oral cavity is the main entrance for two systems crucial to human function and physiology, the gastrointestinal and respiratory systems, and is known as “the intersection of dentistry and medicine” and “the window to general health.” It also contains some of the most diverse and vast flora in the human body. As a result, certain infections in the oral cavity may result in infection foci that could harm the body as a whole.
The mouth cavity contains more than 500 different types of bacteria, viruses, fungi, and protozoa. In the microenvironment of the oral cavity, numerous microorganisms cling to the teeth, the gingival sulcus, the tongue, and the buccal mucosa. Atypical organisms start to predominate when a local or systemic illness process or concurrent medication use affects this overall pattern, and some normal organisms with a benign nature may turn pathogenic. Depending on the patient’s age, the eruption or loss of teeth, or the presence of other active conditions, the oral cavity’s microenvironment may alter (e.g., caries, periodontal disease). The quantity and composition of the oral flora might also change due to systemic changes, such as pregnancy or drug use. These modifications result from changes in salivary fluid flow and composition as well as salivary levels and defence component activity (such as immunoglobulins and cytokines).
Periodontitis, one of the most common chronic bacterial dental infections, affects the tooth’s supporting tissues. The host’s reaction to the infection has a considerable impact on the scope and severity of the sickness. Systemic illnesses mostly affect the proper functioning of immune and inflammatory processes, which might alter the severity of periodontitis.
Oral foci of infection have a substantial effect on a person’s overall health and are linked to long-term disorders like cardiovascular disease, diabetes mellitus, kidney disease, lung disease, and even difficulties from pregnancy.
There is mounting evidence that oral microbes contribute to several systemic disorders. The majority of people overlook or are unaware of the possibility that having poor dental health could seriously harm their general health. Therefore, to avoid serious consequences, both general healthcare providers and oral-care physicians must make maintaining good dental hygiene through patient education and giving the finest oral care their top priority.
Bacterial Endocarditis
A bacterial infection of the endocardium is known as bacterial endocarditis (BE), sometimes known as infective endocarditis. Particularly in persons with impaired immune systems, it is regarded as extremely morbid and fatal. High-risk patients include those with artificial heart valves, those with structural or congenital heart disease, and those who misuse intravenous medications. People with congenital heart defects and, in particular, those with valvular heart disease of rheumatic origin are most susceptible to BE.
Etiology and pathogenesis
BE is significantly influenced by oral infections and oral bacterial flora. Bacteremia can develop not only following invasive operations but also following standard oral hygiene practices like brushing and flossing your teeth, as well as even when you’re chewing. It’s interesting to note that according to the American Heart Association, the degree of bacteremia following a tooth extraction is comparable to that brought on by cleaning or flossing your teeth. Despite having brief durations and a modest bacterial burden, these bouts of bacteremia can occasionally continue up to an hour. However, there is debate concerning the severity or persistence of bacteremia linked to oral or dental aetiology.
The primary mechanism for the development of BE is thought to be the intricate interaction of the bloodstream pathogen with matrix molecules and platelets at areas of endocardial cell injury. Most often, the first stages of BE start in a mass composed primarily of platelets and fibrin, which is initially free of microbes but is prone to becoming colonised by them. However, the majority of bacteremia’s are temporary, self-limited, and do not cause systemic problems.
90% of BE cases are caused by Staphylococcus, Streptococcus, and Enterococcus species. Oral streptococci, which are a member of the viridians group, are a host for oral flora. These microbes, which are a component of dental plaque, may produce bacteremia through regular behaviours like chewing or teeth brushing. Bacteremia can also be brought on by dental extractions or other dental operations.
Dental considerations
If no treatment is started, BE is a deadly condition in 30% of instances. In most cases, an extended course of antibiotic therapy administered intravenously (with benzylpenicillin and gentamicin) is recommended. Penicillin is not used in the treatment of staphylococcal endocarditis; vancomycin is. The infected valve may need to be replaced in extreme circumstances, such as prosthetic valve endocarditis.
Prophylaxis against BE with antibiotics is still debated. Some studies report that antibiotics administered before a dental procedure may reduce the frequency or duration of bacteremia, while others fail to support this statement.
The American Heart Association advises antibiotic prophylaxis for patients who are most likely to experience negative effects from BE. Antibiotic prophylaxis is necessary before dental operations that affect the oral mucosa, gingival tissues, or the periapical region of a tooth. The table below lists recommended antibiotic regimens for dental patients who are at high risk for BE. Patients who have experienced anaphylaxis, angioedema, or urticarial after taking penicillin or ampicillin are not advised to take cephalosporins.
Diabetes Mellitus
Diabetes mellitus (DM) is characterised by a breakdown in glycemic regulation brought on by either systemic insulin resistance (type 2 DM) or a lack of insulin secretion (type 1 DM), which leads to protracted exposure to hyperglycemia. The heart, eyes, kidneys, and peripheral nerves are all adversely impacted by prolonged hyperglycemia, which is the primary cause of DM-related problems. Additionally, oral infections are mentioned as one of the main DM side effects.
Etiology and pathogenesis
Hyperglycemia, which causes the creation of advanced glycation end products, is the cause of oral problems associated with DM. From a systemic perspective, advanced glycation end products are to blame, leading to an increase in cytokine production, localised inflammation, and connective tissue degradation. Localized inflammation in the mouth cavity affects glycemic management on a systemic level, making it more difficult since it increases the risk of infection. Due to decreased immunologic processes, such as chemotaxis, phagocytosis, and microbicidal properties of polymorph nuclear neutrophils, macrophages, monocytes, and T lymphocytes, DM patients are more susceptible to infections. Insulin resistance, dyslipidemia, and hypertension are additional processes underlying the chronic consequences of DM, in addition to hyperglycemia and immunological dysfunction.
Dental considerations
Diabetic patients may potentially have greater rates of alveolar bone loss, abscess formation, and subpar healing because DM is a risk factor for periodontitis. Although studies demonstrate that patients with well-controlled diabetes have no increased risk of periodontitis compared to healthy individuals, diabetic patients do have at least a threefold greater risk of the condition than healthy patients. DM oral consequences include dental decay, dry mouth, Candida-related lesions, and glossitis.
According to several studies, over 52% of people with diabetes and periodontitis also have oral Candida infections. Patients with type 2 DM who are not well controlled are three times more likely to develop periodontal disease. HbA1c and fasting blood glucose levels are observed to be greater in periodontitis patients than in periodontal healthy people. People who have severe periodontitis are at a much higher risk. Appropriate periodontal care improves HbA1c levels by 0.4-0.6%, implying that periodontal care is linked to better glycemic management.
The combination care of persons with diabetes and periodontitis requires close clinical teamwork between the dental and medical teams. Overall, it is important to recognise that current diabetic care must include both the management and prevention of oral as well as systemic problems connected to DM. To manage patients in the best way possible, patients may benefit from an interdisciplinary approach involving general healthcare physicians and dental specialists.
Conclusion
The goals of medical and dental healthcare providers are the same: to improve patients’ health and lower morbidity and mortality rates.
Diabetes mellitus, cardiovascular, and cerebrovascular illnesses have all been extensively researched for their potential links to dental health. Evidence-based medicine demonstrates that oral infections may contribute to the development of various systemic disorders and may also have an impact on disease progression. On the other hand, the findings of research on the impact of treating oral disorders on systemic conditions seem debatable.
Physicians should collaborate more since it is preferable to avoid illness than to treat it in the healthcare system. The majority of patients may not be aware that oral health issues can have a considerable impact on their overall health, and that treating any concomitant conditions may be sufficient to avoid serious or even potentially fatal medical consequences.
To demonstrate a stronger link between oral health and systemic illnesses, however, additional study is needed in this area.